
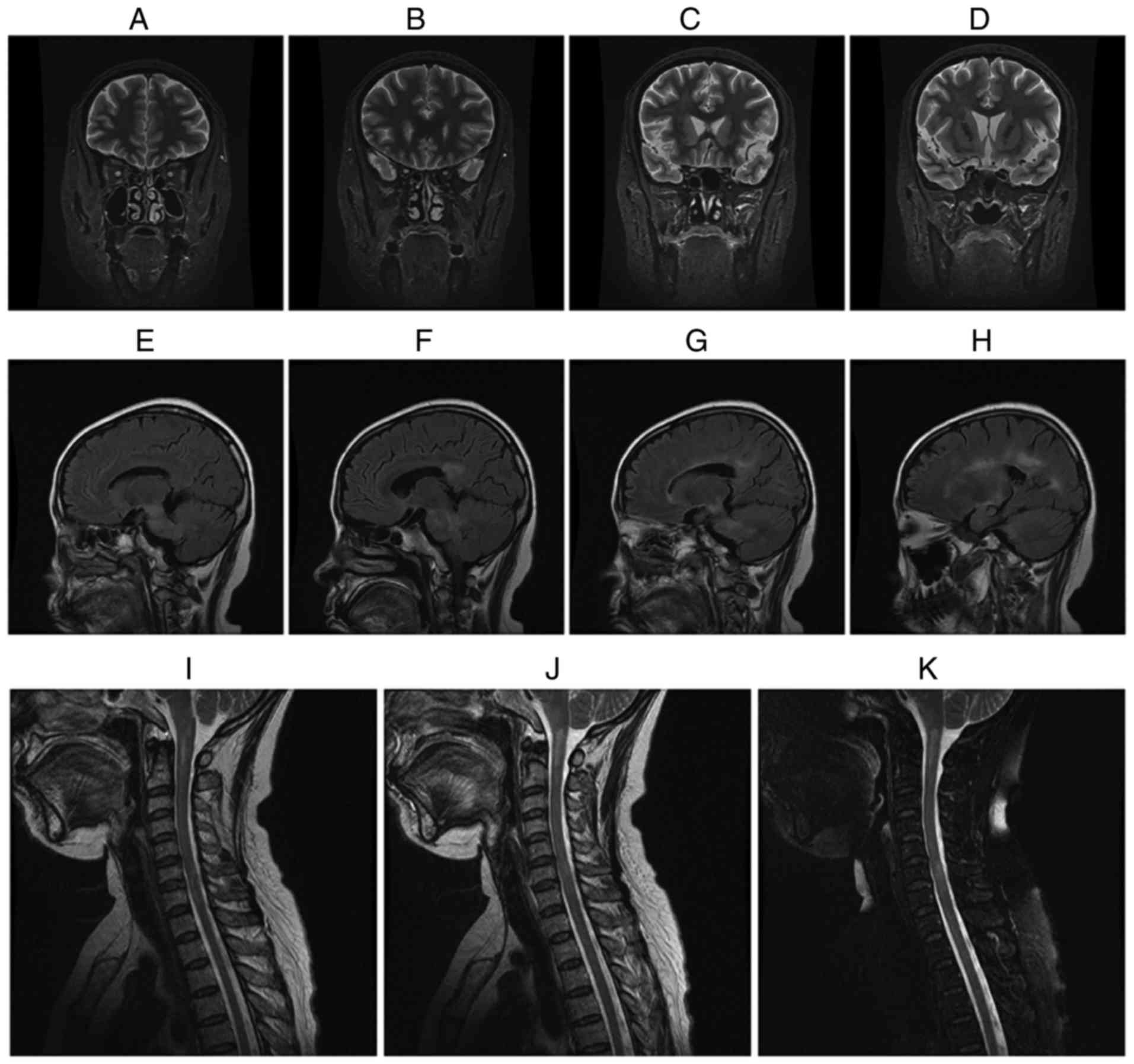
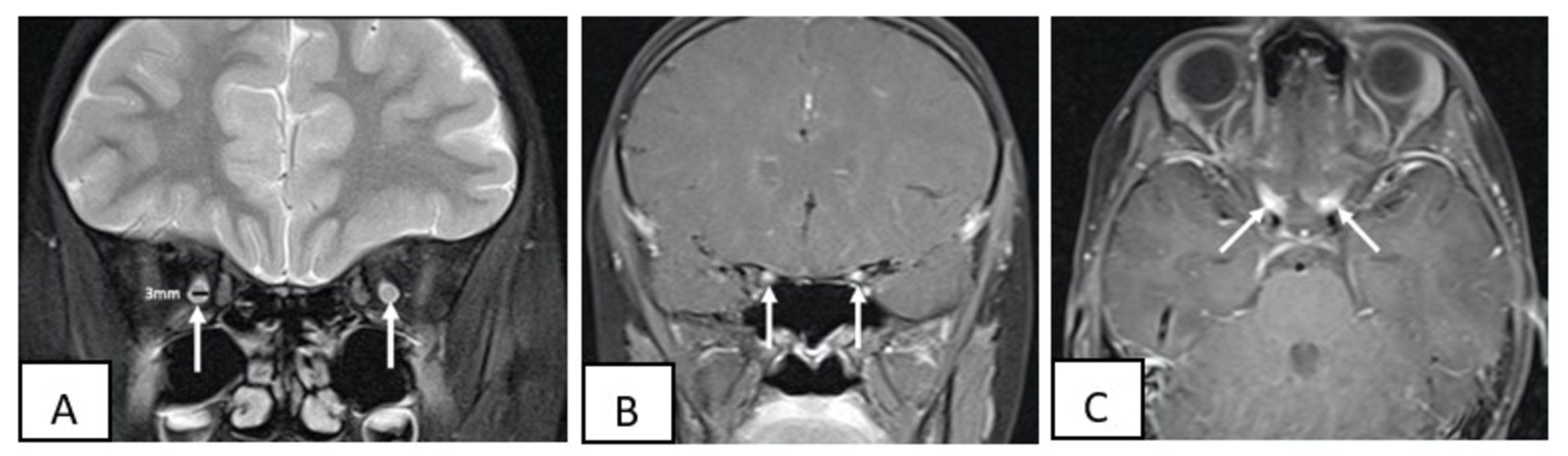
However, aroundĦ0% to 80% of patients with acute optic neuritis have nonspecific findings in the CSF such Puncture, is done to exclude other causes of visual loss in atypical cases. Further diagnostic testing, such as lumbar MRI of the brain and orbits with gadolinium contrast provide aīetter assessment of the diagnosis in most cases. Because important findings on funduscopic examination help differentiate typicalįrom atypical cases of optic neuritis, an ophthalmologic examination can be considered in In general, optic neuritis is a clinical diagnosis based on the history and examinationįindings. 3 T-cell activation leads to the release of cytokines and other inflammatory agents.ī-cell activation against myelin basic protein is not seen in peripheral blood but can beĭemonstrated in the CSF of patients with optic neuritis. Systemic T-cell activation is identified at symptom 2 It is believed that the demyelination in optic neuritis is immune-mediated, but theĮxact targeted antigens remain unknown. It is highly associated with MS, and it is the presentingįeature in 15% to 20% of these patients and occurs in 50% of them at some time during their illness. Optic neuritis is defined as an inflammatory, demyelinating condition that causes acute, Tapering dose of prednisone over 4 weeks with planned follow-up with ophthalmology and Remarkable but not complete vision recovery in the right eye. Byĭay of discharge, our patient had complete restoration of vision in the left eye with Within 48 hours, his vision and eye pain had shown significant improvement. The patient was started on methylprednisolone 1 g every 24 hours for a total of 5ĭays/doses. Virus RNA PCR and serum severe acute respiratory syndrome coronavirus 2 IgG antibodies wereĭetected. Nasopharyngeal severe acute respiratory syndrome Immunological panel including IgG, ANA, JO-1, Anti-NMOĪb, SS-A, and SS-B were also negative. Viral panel including Epstein–Barr virus, HIV, andĬytomegalovirus was negative. Myelin oligodendrocyte glycoprotein (MOG) was detected withĪ titer of 1:160 (<1:10). Mg/dL (12-60 mg/dL) with negative gram stain. White blood cell count of 3 cells/µL (0-5 cells/µL), red blood cell count of 6.0 cells/µL,Īlbumin 23.3 mg/dL (8-42 mg/dL), glucose of 88 mg/dL (40-70 mg/dL), and total protein 50 Lumbar puncture was done with nonspecific findings of colorless cerebrospinal fluid (CSF), Brain MRI showedĮnhancement in the right more than the left optic nerve suggestive of optic neuritisĪlthough no other abnormalities were noted in brain, cervical, or thoracic spine ( Figures 1 1 - -3).
Laboratory findings including complete blood count, comprehensive metabolic panel, urineĪnalysis, and drug screen were all negative and/or unremarkable. Left eye’s vision was with a superior arcuate visual field defect and 20/30 acuity. Loss was noted in the right eye with acuity 20/200 along with relative afferent pupil areaĭefect. On formal visual fields examination, a global vision Vision to the extent of complete vision loss. Right eye that had progressed to his left eye along with worsening bilateral blurring of One week prior to his admission, he reported developing pain in his Required hospitalization for his respiratory illness nor medications including He was quarantined at his home and treated symptomatically with improvement he never Polymerase chain reaction (PCR) after developing symptoms of shortness of breath and cough. Had tested positive for coronavirus disease 2019 (COVID-19) virus by nasopharyngeal Two weeks prior to onset of eye and vision symptoms, he A 44-year-old Hispanic male patient with no past medical history presented from clinic withīilateral eye pain and vision loss.


 0 kommentar(er)
0 kommentar(er)
